Covid-19 Crisis
and Rich Countries
Most of this reasoning was speculative. But by the late summer of 2020, two clear trends were emerging. While parts of Western Europe were enduring a devastating first wave of Covid-19 cases, Africa and south Asia were experiencing a slow-moving, sometimes stalling rate of infection and a comparatively low death toll. Those trends are now being reversed.
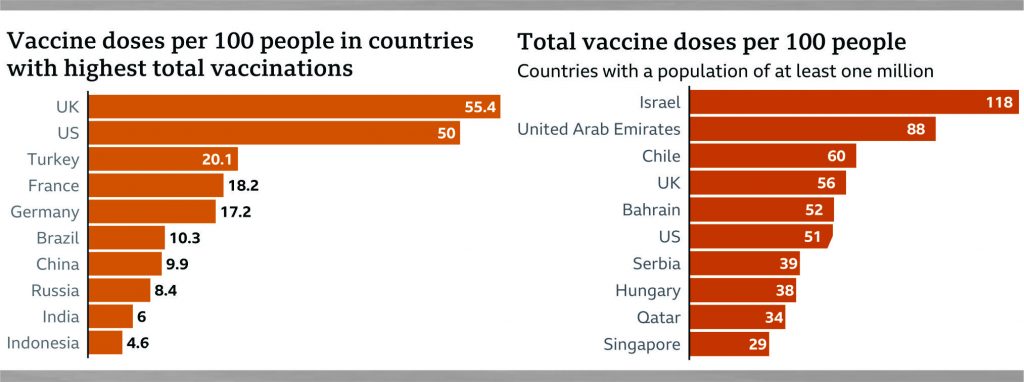
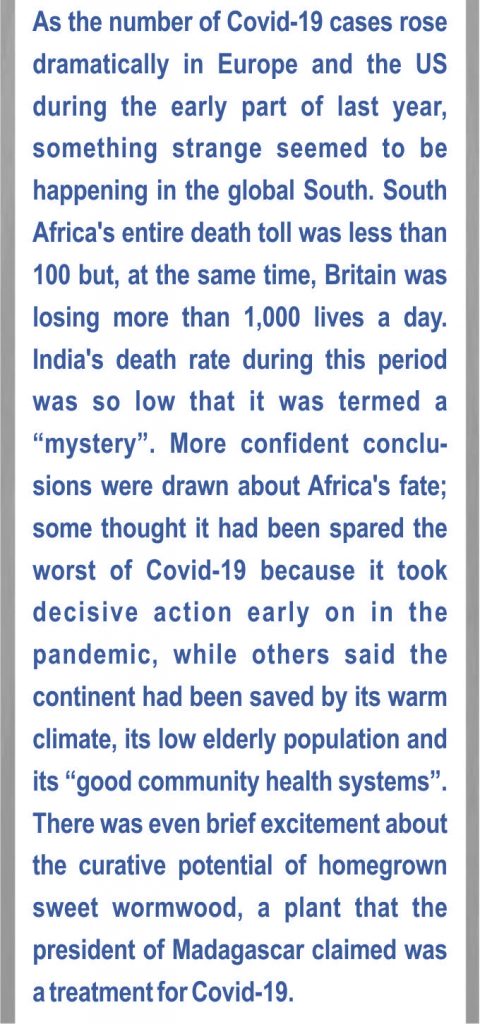 With vaccination programs gaining momentum in the global north, the pandemic in Western countries finally appears to be waning. The opposite is happening in low-income countries. Most can expect no access to either vaccine technology or donations in the near future. Healthcare facilities are overstretched and under-resourced, and data collection is limited, meaning death statistics are unreliable. Most of the world’s people outside rich countries are confronting an extended Covid crisis. Indeed, for several countries there is no way of estimating when the pandemic will be over. Instead, what lies ahead is an open-ended stretch of uncertainty, as populations try, and inevitably fail, to coexist with this virus.
With vaccination programs gaining momentum in the global north, the pandemic in Western countries finally appears to be waning. The opposite is happening in low-income countries. Most can expect no access to either vaccine technology or donations in the near future. Healthcare facilities are overstretched and under-resourced, and data collection is limited, meaning death statistics are unreliable. Most of the world’s people outside rich countries are confronting an extended Covid crisis. Indeed, for several countries there is no way of estimating when the pandemic will be over. Instead, what lies ahead is an open-ended stretch of uncertainty, as populations try, and inevitably fail, to coexist with this virus.
For every measure that placed Africa and South Asia in a good position at the start of the pandemic, there is another that undermines it. There are indeed strong community health systems in parts of West Africa, a legacy of the Ebola crisis. Those networks can raise awareness, but without the ability to test for Covid-19, they are unable to get a clear idea of infection rates. The same applies to mortality figures. In rural areas, many people do not have access to large hospitals, and some deaths are not formally recorded. The fear of social stigma that a Covid-19 diagnosis can carry means some people bury their deceased relatives in haste, without getting a diagnosis or alerting family and social networks.
 Instead of reliable data, those of us with family and friends in low-income countries have hushed, anecdotal evidence that does not correspond to official accounts. We measure waves by keeping track of what we hear; we learn to recognise the signs. Whenever relatives tell us of a quick illness or a hushed-up death, the deceased person is added to an informal mental tally of Covid-19 cases.
Instead of reliable data, those of us with family and friends in low-income countries have hushed, anecdotal evidence that does not correspond to official accounts. We measure waves by keeping track of what we hear; we learn to recognise the signs. Whenever relatives tell us of a quick illness or a hushed-up death, the deceased person is added to an informal mental tally of Covid-19 cases.
Successfully defeating the virus depends on having solid numbers and a dashboard of data. Without those, scientists are fighting this disease in the dark, as Michelle Gayer, director of emergency health at the International Rescue Committee, recently told the business publication Quartz. When a virus is allowed to quietly spread and scientists don’t have the data to map its trajectory, it is difficult to tell what is actually happening until a traumatic spike in death rates sheds light on the number of cases. This is the current reality in India, and while I do not wish to be a doom-monger, it seems likely this will soon be the case in other countries too.
 A brief survey of a few of the largest African countries by population shows how volatile the situation still is. South Africa and Ethiopia remain on the UK’s red list and are in varying stages of lockdown while their governments cobble together vaccine programs. Kenya has wobbled out of another lockdown but maintains a strict curfew and remains on the red list. Egypt has truncated the school year and appears to be heading for the peak of its third wave. The main coping strategies available to these countries are Sisyphean cycles of lockdowns and easing. These buy governments time and reduce the pressure on limited healthcare facilities, but they ravage the economy in the process. In poorer countries where state support is limited, lockdowns can be as deadly as the virus itself, because they remove people’s ability to make a living.
A brief survey of a few of the largest African countries by population shows how volatile the situation still is. South Africa and Ethiopia remain on the UK’s red list and are in varying stages of lockdown while their governments cobble together vaccine programs. Kenya has wobbled out of another lockdown but maintains a strict curfew and remains on the red list. Egypt has truncated the school year and appears to be heading for the peak of its third wave. The main coping strategies available to these countries are Sisyphean cycles of lockdowns and easing. These buy governments time and reduce the pressure on limited healthcare facilities, but they ravage the economy in the process. In poorer countries where state support is limited, lockdowns can be as deadly as the virus itself, because they remove people’s ability to make a living.
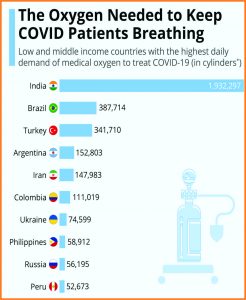
The outcome is not only sporadic flare-ups or confined challenges, but an entire population trapped by and condemned to live with the virus. The best-case scenario is that governments are able to contain a high peak of cases through lockdowns, while lives and livelihoods are lost to economic restrictions. The worst is the kind of explosion we are seeing in India. Some observers estimate that the virus will kill more people in 2021 than it did in 2020.
Which brings us to what can and should be done. That the pandemic is not playing out in poorer countries with the same virulence we saw in Western countries does not mean there aren’t slow and deadly fires smouldering, which could yet grow into an inferno. There is a delay built into our responses to Covid-19, both at home and abroad. As Western governments learned from the first wave, by the time the heavy death tolls are upon us, it is already too late. By the time the world had seen the images from India showing mass cremations, the country was already embroiled in a crisis. Those images prompted Joe Biden to reverse his position and pledge to send a “whole series of help”. I’d wager that if the world had been exposed to similar images from other countries, it would have become untenable for the West to maintain vaccine apartheid.
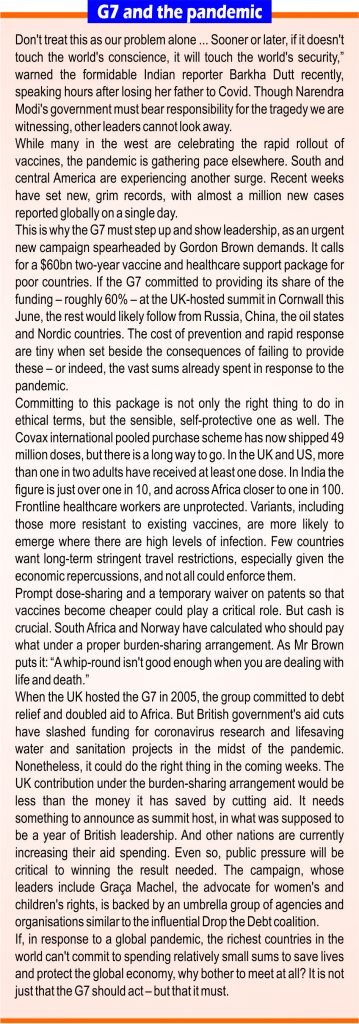
 But we shouldn’t have to wait for images like those to spur action. What is required is something far more ambitious than vaccine donations. The world needs a global logistical exercise, a sort of Marshall Plan that would provide financial support, expert manpower and medical technology. In the US, Democratic senators, progressives, NGOs and an alliance of 175 former world leaders and Nobel laureates have come together to apply pressure on Biden to waive intellectual-property protections on vaccines. As the virus recedes in the West, now is the time to apply this kind of pressure on leaders to deliver the South from its almost certain fate. By the time the real numbers of deaths and infections in poorer countries become clear, it will be far too late for many people.
But we shouldn’t have to wait for images like those to spur action. What is required is something far more ambitious than vaccine donations. The world needs a global logistical exercise, a sort of Marshall Plan that would provide financial support, expert manpower and medical technology. In the US, Democratic senators, progressives, NGOs and an alliance of 175 former world leaders and Nobel laureates have come together to apply pressure on Biden to waive intellectual-property protections on vaccines. As the virus recedes in the West, now is the time to apply this kind of pressure on leaders to deliver the South from its almost certain fate. By the time the real numbers of deaths and infections in poorer countries become clear, it will be far too late for many people.
The writer is the author of “We Need New Stories: Challenging the Toxic Myths Behind Our Age of Discontent”
 Jahangir's World Times First Comprehensive Magazine for students/teachers of competitive exams and general readers as well.
Jahangir's World Times First Comprehensive Magazine for students/teachers of competitive exams and general readers as well.